10 Must-Know Facts About Home Oxygen Therapy
Home oxygen isn’t a last resort—it’s a science-backed lifeline that can help you reclaim energy, sleep, and independence when used correctly. It is a vital treatment for those with chronic respiratory conditions like COPD, pulmonary fibrosis, and severe asthma. It helps maintain healthy blood oxygen levels, improving organ function, sleep, and daily activities. Here’s what you need to know:
-
When is it needed? Recommended when blood oxygen levels drop below 88%. Normal levels are 95% or higher.
-
How does it help? Delivers oxygen-enriched air through devices like nasal cannulas or masks. It supports organ function but doesn’t cure the underlying condition.
-
Safety first: Always use oxygen therapy under a doctor’s prescription. Avoid smoking as it poses severe fire risks.
-
Types of systems: Choose from compressed gas, liquid oxygen, or portable oxygen concentrators based on your lifestyle and medical needs. Liquid oxygen systems are less common in India for home use, as most families rely on oxygen concentrators or compressed cylinders for convenience and affordability.
-
Costs in India: Costs in India: New oxygen concentrators cost ₹49,000–₹1,65,000; quality used/refurbished models are available for ₹25,000–₹1,10,000.
Rentals typically start at ₹3,500–₹4,500 per month for standard 5 LPM concentrators.
ICU-grade or high-flow units may rent from ₹5,000–₹15,000 per month, depending on features and location. -
Fire safety: Keep equipment 3 metres away from flames and heat sources. Install smoke detectors and follow strict safety rules.
-
Maintenance: Clean tubing weekly, replace components as needed, and schedule professional inspections.
-
Warning signs: Watch for symptoms like breathlessness, confusion, or bluish skin. Use a pulse oximeter to monitor levels.
-
Compliance matters: Stick to prescribed flow rates to avoid complications like hypoxia or oxygen toxicity.
-
New advancements: AI-powered devices, high-flow systems, and remote monitoring are making oxygen therapy more efficient and user-friendly.
-
Insurance/Finance: Most health insurance policies in India do not cover home oxygen equipment. Renting is a cost-effective option for most families.
Quick Tip: Always consult your doctor for the right oxygen system and settings. Follow safety guidelines to ensure effective and safe therapy.
Things to Know When Using Oxygen Therapy
1. What Oxygen Therapy Does and Its Limits
Home oxygen therapy helps raise blood oxygen levels, ensuring vital organs get the oxygen they need when lung function is impaired [4]. Think of it as a lifeline for maintaining healthy oxygen levels when the body struggles to do so on its own.
The therapy works by delivering oxygen-enriched air through devices like nasal cannulas, face masks, or tracheotomy tubes. This provides a higher oxygen concentration than normal air, compensating for the lungs' reduced ability to extract enough oxygen [1].
"Supplemental oxygen therapy helps people with COPD, COVID-19, emphysema, sleep apnea and other breathing problems get enough oxygen to function and stay well. Low blood oxygen levels (hypoxemia) can damage organs and be life-threatening." - Cleveland Clinic [1]
In India, oxygen therapy is most often used for conditions like Chronic Obstructive Pulmonary Disease (COPD), Post-Tuberculous Obstructive Airway Disease, and Interstitial Lung Disease (ILD). A study in Delhi with 97 patients revealed that COPD accounted for 49.48% of long-term oxygen therapy cases, followed by post-tuberculous conditions at 20.6% and ILD at 12.37% [7]. These figures highlight the importance of tailoring oxygen therapy to specific medical conditions.
However, it's equally important to understand the therapy's limits. Oxygen therapy supports organ function and helps alleviate symptoms, but it does not cure the underlying condition [1]. If your blood oxygen levels are already normal, oxygen therapy won't reduce breathlessness and may not be necessary [4].
The therapy is most beneficial for patients whose blood oxygen levels fall below 88% [1]. If your oxygen saturation is above 95%, using extra oxygen is usually unnecessary and can be harmful. Always use oxygen therapy under medical supervision.
For the best results, studies suggest using supplemental oxygen for at least 18 hours a day [8]. This highlights its role as a consistent, daily treatment rather than a temporary fix.
"Oxygen helps our body turn food into energy, which we need for growth, repair and movement." - Asthma + Lung UK [3]
When used as part of a broader treatment plan, oxygen therapy can boost energy, improve sleep quality, and enhance overall well-being by ensuring vital organs receive adequate oxygen. However, it must always be prescribed by a healthcare professional based on specific tests that confirm its necessity [4].
Long-term use of oxygen therapy - at least 15 hours daily - has been shown to improve life expectancy in individuals with severely low oxygen levels [3]. This makes it a critical treatment option when used correctly and consistently under medical supervision. Up next, learn how to properly set up and use oxygen equipment for safe and effective daily use.
2. How to Set Up and Use Oxygen Equipment
Properly setting up oxygen equipment is essential to ensure you receive the prescribed oxygen safely and effectively. Each step requires attention to detail and strict adherence to your healthcare provider's guidance.
Initial Setup and Safety Checks
Before you begin, check the oxygen gauge on your tank to confirm there's enough oxygen available for use [9]. For portable oxygen concentrators, follow your doctor's instructions or device manual to switch on the device correctly [9].
Place your oxygen equipment in a well-ventilated area, away from heat sources, open flames, or direct sunlight [13][15]. Oxygen cylinders should be stored upright and secured to prevent tipping. Keep the area free of flammable materials [14][15].
Flow Rate Configuration
Set the flow rate as prescribed by your doctor, which is usually between 1–15 L/min. Check the setting on the flow meter to ensure accuracy [9][10].
"Do not self-adjust your oxygen flow rate without consulting your doctor." - American Lung Association [11]
To confirm oxygen is flowing, feel for air movement from the device's exit ports [10]. If you're unsure, place the cannula in a glass of water; bubbles will indicate active oxygen flow [9].
Tubing and Cannula Placement
Carefully attach the tubing to your equipment, ensuring there are no kinks that could block airflow [9][10]. Securely connect the nasal cannula or face mask, positioning it comfortably. For nasal cannulas, the prongs should sit gently in your nostrils.
To prevent dryness, apply a water-based lubricant around your nostrils [6][9]. Clean the tubing regularly with alcohol based santizer to maintain hygiene [14].
Equipment Maintenance and Storage
Regular upkeep keeps your equipment functioning efficiently and reduces the risk of infections. Clean the internal filter of your concentrator at least once a month [14]. Keep all equipment free from dust and avoid using it in dusty environments [14][15]. Never cover oxygen cylinders with cloth or plastic materials [15].
Inspect the cylinders, regulators, and tubing frequently for any signs of damage or leaks [12]. Always check the pressure gauge before use to ensure there's enough oxygen in the cylinder [12]. If you use electric concentrators, ensure nearby electrical equipment is properly grounded [15].
Emergency Preparedness
Inform your family members and building security staff that oxygen equipment is in use, so they can assist in an emergency[6][9]. Create a backup plan for power outages or equipment malfunctions, especially if your setup relies on electricity [13].
It's crucial to remember that oxygen supports combustion, which means it can make materials burn much faster in an oxygen-rich environment [15]. While oxygen itself is not explosive, following safety guidelines will help protect you and your household from potential risks.
3. Fire Safety Rules for Indian Homes
Ensuring fire safety is a critical part of using oxygen therapy at home. While proper setup and maintenance are essential, taking precautions against fire risks is equally important. Oxygen, while life-saving, can significantly increase the risk of fire when mixed with common household hazards.
"Oxygen is like fuel to fire. So, an oxygen-rich environment poses threat in areas closer to fire & smoke." [16]
Maintaining Safe Distances
Always keep your oxygen concentrator at least 3 metres away from open flames, such as gas stoves, candles, diyas, and incense burners [16]. This rule also applies to the concentrator's accessories, like tubing and masks. If your home has limited space, consider moving the equipment to a room with fewer potential fire hazards.
Additionally, avoid using electric appliances like hair dryers, electric razors, or even electric toys near the oxygen concentrator [16]. This is especially important during festivals when homes often have extra electrical decorations. By following these precautions, you reduce the risk of fire and create a safer environment.
Household Products to Avoid
Certain household items can increase fire risks when used near oxygen equipment. Avoid aerosol sprays, paints, cleaning solvents, and petroleum-based products [16]. If you use cosmetics, switch from oil-based products and petroleum jelly to water-based alternatives during oxygen therapy [16].
Essential Safety Installations
Beyond avoiding hazardous products, installing safety measures is crucial. Place smoke detectors in any room where oxygen therapy is used [16]. Ensure the oxygen concentrator is properly grounded and try to never plug it into extension cords or power strips [16]. Clearly post "No Smoking" signs and make sure everyone in the household understands and follows this policy [17].
Storage and Positioning Guidelines
Store oxygen cylinders upright in a stable, secure position. Keep them in a clean, uncluttered, and well-ventilated area [16][19].
The dangers of oxygen-related burns are severe. As Dr. Lucy Wibbenmeyer explains, "Individuals incurring burns while using oxygen are more likely to die than similar burns" [18]. This underscores the need for strict adherence to fire safety measures when using oxygen therapy at home.
4. 3 Main Types of Home Oxygen Systems
Selecting the right home oxygen system is essential for safe and effective oxygen therapy. The choice depends on your medical needs, lifestyle, and mobility. The three primary types of systems are compressed gas systems, liquid oxygen systems, and portable oxygen concentrators (POCs). Each has unique features to meet different requirements.
Compressed Gas Systems
These systems include a stationary concentrator for home use and smaller portable tanks for when you’re on the go[21]. The stationary unit connects upto 50-foot tubing, giving you freedom to move around your home. Portable tanks, which can either be delivered pre-filled or refilled overnight using the concentrator, provide oxygen for outdoor activities.
Liquid Oxygen Systems
Liquid oxygen systems combine a stationary reservoir with a refillable portable tank for outdoor use[21]. One litre of liquid oxygen expands to about 860 litres of gas[20], offering a higher oxygen concentration and longer usage times between refills. This makes them ideal for patients who are active and spend significant time away from home. Liquid oxygen systems are less common in India for home use, as most families rely on oxygen concentrators or compressed cylinders for convenience and affordability.
Portable Oxygen Concentrators (POCs)
POCs are compact, electric devices designed for mobility. They can function as both portable and, in some cases, stationary systems[21]. Powered by electricity or rechargeable batteries, they are easy to transport and approved for air travel. Most portable oxygen concentrators allow tubing lengths up to 15 feet, though shorter tubing is recommended for optimal mobility and oxygen flow.
|
System Type |
Best For |
Key Advantage |
Main Limitation |
|---|---|---|---|
|
Compressed Gas Systems |
Patients who stay home but go out occasionally |
Combines home and portable oxygen supply |
Portable tanks need frequent refills |
|
Liquid Oxygen Systems |
Active individuals and/or frequently outdoors |
High oxygen concentration with longer use |
Costs about four times more than concentrators[20] |
|
Portable Oxygen Concentrators |
Travellers and those with active lifestyles |
Full mobility and airline approval |
Limited to tubing length and most POCs do not have continuous Flow |
Cost Overview
Costs in India: New oxygen concentrators cost ₹49,000–₹1,65,000; quality used/refurbished models are available for ₹25,000–₹1,10,000.
Rentals typically start at ₹3,500–₹4,500 per month for standard 5 LPM concentrators.
ICU-grade or high-flow units may rent from ₹5,000–₹15,000 per month, depending on features and location.[20].
Efficiency and Usage
Studies indicate that oxygen concentrators are more cost-effective and safer for patients needing oxygen for over 1.4 hours a day compared to compressed gas cylinders[20]. Additionally, patients using liquid oxygen tend to spend more time outdoors and use oxygen for longer periods than those relying on concentrators[20].
When choosing a system, consider factors like your prescribed oxygen flow rate, how often you leave home, your ability to manage the equipment, and the layout of your home. Discuss these options with your healthcare provider to determine the best fit for your needs. Up next, find out why sticking to your prescribed oxygen flow rate is so important for effective treatment.
5. Why Following Prescribed Flow Rates Matters
Your prescribed oxygen flow rate isn't just a number - it's a carefully calculated medical guideline tailored to your health needs. Sticking to this rate is essential for ensuring your oxygen therapy works effectively while minimising potential risks.
The Science Behind Flow Rates
Doctors determine your flow rate based on your unique medical condition, activity level, and target oxygen saturation levels. For most individuals, maintaining oxygen saturation between 90% and 92% is crucial to avoid tissue hypoxia while also preventing complications from receiving too much oxygen [5]. This balance ensures your organs receive adequate oxygen without overloading your system.
Risks of Incorrect Flow Rates
Using the wrong flow rate can lead to serious health issues. If the rate is too low, you risk hypoxia, which can strain vital organs. On the other hand, excessive oxygen (hyperoxia) can suppress breathing in some patients. For those with chronic obstructive pulmonary disease (COPD), unchecked oxygen delivery can worsen hypercapnia - a dangerous rise in carbon dioxide levels in the blood [5][24].
Different Delivery Methods and Their Flow Rates
The effectiveness of oxygen therapy also depends on the delivery method and its corresponding flow rate:
-
Nasal cannulas: Typically require 1 to 6 litres per minute [22].
-
Simple masks: Operate best at 6 to 10 litres per minute [22].
-
Non-rebreather masks: Demand the highest flow rates, ranging from 10 to 15 litres per minute [22].
Recognising Oxygen Toxicity
Prolonged exposure to oxygen levels above 50% can lead to toxicity. Symptoms to watch for include chest pain, shortness of breath, dizziness, muscle spasms, nausea, and vision disturbances [1]. Just as regular maintenance ensures your oxygen equipment functions safely, adhering to prescribed flow rates protects your health and reduces the risk of these complications [5].
How to Maintain Your Prescribed Settings
Always ensure your oxygen flow rate matches the prescribed settings. Avoid making adjustments on your own, and regularly check that your equipment is functioning correctly. Make sure the tubing is free of kinks and that the flow meter - controlled by a steel ball inside a glass cylinder - is set to the correct rate [22][23].
For added safety, use a pulse oximeter to monitor your oxygen saturation levels and review your prescription annually with a respiratory specialist or whenever your health condition changes [25]. Regular monitoring and adherence to your prescribed flow rate are essential for safe and effective oxygen therapy.
6. Equipment Maintenance Schedule
Taking care of your oxygen equipment is crucial for both safety and long-term reliability. With proper maintenance, oxygen systems can serve you well for years. For instance, some portable concentrators can last up to 8 years if used for less than 8 hours daily [27].
Daily Maintenance Tasks
Start your day by giving your equipment a quick inspection. Check for visible damage, including cracks or dents in the tubing, and ensure all connections are secure. Look at your nasal cannula or mask for any signs of wear, such as cracks, holes, mould, or discolouration, which may affect oxygen delivery. If you're using a humidifier, confirm that it’s working properly and filled with distilled water.
Weekly Cleaning Routine
To prevent bacterial and mould buildup, clean your nasal cannula or mask weekly using mild soap and warm water. Rinse thoroughly and let it air dry. Use the same method to clean your oxygen tubing and other accessories.
For humidifiers, wash them with warm water and mild soap, rinse well, and disinfect weekly using a vinegar-water solution. This routine ensures clean oxygen delivery and reduces the risk of contamination.
Monthly Replacement Schedule
Some parts of your equipment need regular replacement to maintain hygiene and performance. Replace your humidifier every month and consult your equipment manual for instructions on replacing filters or other components. Neglecting these replacements can affect oxygen flow and concentration levels.
Essential Maintenance Checklist
|
Component |
Cleaning Frequency |
Replacement Frequency |
|---|---|---|
|
Nasal Cannula/Mask |
Once a week with mild soap and water |
Replace if damaged/discolouration |
|
Humidifier |
Weekly cleaning and vinegar disinfection |
Replace monthly |
|
Oxygen Tubing |
Weekly cleaning with mild soap and water |
Replace when worn or damaged |
Following this checklist helps ensure your equipment delivers oxygen efficiently and avoids unnecessary breakdowns.
Deep Cleaning Procedures
Once a month, carry out a deep cleaning using a warm water and vinegar solution. This helps remove mineral deposits and biofilm without damaging sensitive components. Make sure all parts are completely dry before reassembling to prevent moisture-related issues.
Battery and Electrical Checks
If you use a portable concentrator, regularly inspect the battery’s condition and clean the battery contacts to maintain efficient charging. Also, check power cords for any signs of fraying or damage, and ensure all electrical connections are secure.
Professional Service Requirements
While daily and monthly maintenance is essential, don’t skip professional inspections. Follow the manufacturer’s recommendations and schedule routine check-ups with a qualified technician. These inspections can catch potential problems early and ensure your equipment continues to deliver oxygen safely.
When not in use, store your equipment in a cool, dry place to extend its lifespan and keep it in good condition.
7. Warning Signs of Low Oxygen Levels
Recognising the signs of low oxygen levels can be crucial for your health. When your body isn't getting enough oxygen, it sends out clear signals. Understanding these symptoms and acting swiftly can prevent severe complications.
Physical Symptoms to Watch For
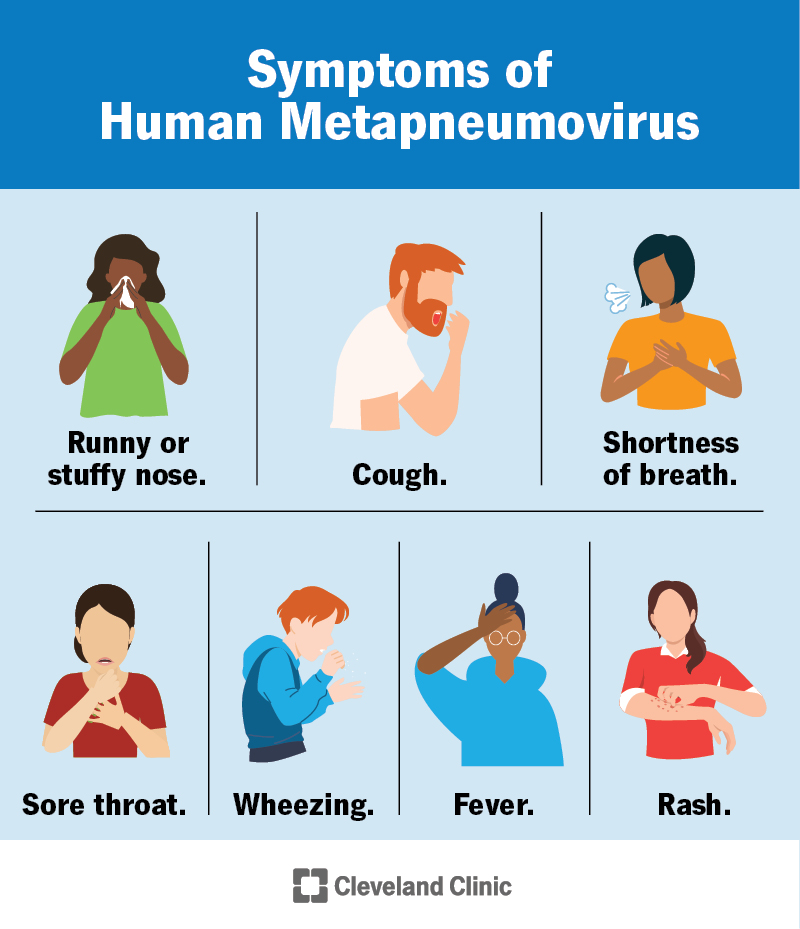
Be alert to symptoms like shortness of breath, a rapid heart rate, restlessness, headaches, anxiety, or sudden confusion. Severe signs include bluish skin, lips, or fingernails (known as cyanosis), extreme restlessness, difficulty breathing, coughing, wheezing, or a slow heart rate [28][29][30].
Why Timing Is Critical
The brain is highly sensitive to oxygen deprivation, with brain cells starting to die within just five minutes of oxygen loss [31]. If hypoxemia (low blood oxygen levels) goes untreated, it can quickly lead to tissue damage. Early detection and immediate action are essential [28][30].
Using a Pulse Oximeter for Early Detection
A pulse oximeter is an effective device for spotting low oxygen levels before severe symptoms develop. Normal readings typically range between 95% and 100%. If your reading falls below 95%, it’s worth consulting a healthcare provider, and levels at or below 92% require urgent medical attention [32][34]. Ideally, oxygen saturation should be between 96% and 99%, with a normal heart rate ranging from 50 to 90 beats per minute [32].
For accurate readings, follow these tips:
-
Remove nail polish.
-
Keep your hand warm and below heart level.
-
Stay still during the measurement.
To monitor trends, check your levels three times a day at consistent times and record the results [32][33][35]. This regular tracking can help you identify any concerning changes early.
When to Seek Immediate Help
If your oxygen saturation drops to 92% or lower, contact your healthcare provider immediately. A reading of 88% or lower is an emergency - get Oxygen at Home or head to the nearest hospital without delay [34]. Pay close attention to symptoms like confusion, rapid heart rate or breathing, or bluish skin, nails, or lips, and act promptly [28][29]. If you have an existing medical condition and notice a sudden worsening of symptoms or new signs of low oxygen, seek emergency care right away. Early intervention is critical to prevent serious complications [37].
Keep in mind that pulse oximeters are most accurate when readings are between 90% and 100%. Their reliability decreases significantly below 80%, and factors like poor circulation, darker skin tones, or movement can affect accuracy. Always consider your physical symptoms alongside the device's readings [35][36].
8. Smoking Risks and Treatment Compliance
Smoking while on home oxygen therapy isn't just risky - it’s a dangerous gamble for you and everyone in your home. The combination of cigarettes and medical oxygen can quickly turn your living space into a fire hazard, with consequences far more severe than many realise.
Why Smoking and Oxygen Are a Deadly Mix
Medical oxygen is almost 100% pure, unlike the 21% oxygen we breathe in regular air [57,59]. This high concentration serves as fuel for fires, making surrounding materials ignite much more easily. Even after the oxygen supply is turned off, enriched oxygen lingers on clothing, hair, and skin, leaving them highly flammable [56,59].
"There is no safe way to smoke when using home oxygen. Even if a person were to stop the oxygen flow and smoke outside, their hair, clothing and skin will still be oxygen-enriched and at risk of catching fire."
– Spokane Valley Fire Department [42]
The statistics are sobering: home oxygen-related fires result in a fatality every four days [39]. Smoking is the primary cause of these incidents, with fires in oxygen-rich environments spreading rapidly and being extremely hard to control [56,61]. Despite these risks, many individuals find it hard to comply with smoking restrictions.
The Struggle to Follow Guidelines
Even with repeated warnings from healthcare professionals, between 14% and 51% of home oxygen users continue to smoke [38]. This highlights the challenge of ensuring compliance. Studies show that heavy smokers often use oxygen therapy less consistently - around 9.3 hours daily, compared to 12.8 hours for non-smokers [55,64].
Research tracking carbon monoxide (CO) levels paints a clear picture: patients with higher CO levels (indicating smoking) used oxygen for an average of 11 hours per day. Non-smokers, however, averaged 12.8 hours, while those with the highest smoking indicators used it for only 9.3 hours daily [45].
Real-Life Consequences
Different countries approach smoking and oxygen therapy differently, and the results are striking. In Sweden, where smoking is strictly discouraged for oxygen therapy users, burn injuries occur at a rate of 85 per 100,000 person-years. Meanwhile, in Denmark - where some patients are permitted to smoke - the rate doubles to 170 per 100,000 person-years [41].
A study of fatal fires in four U.S. states from 2000 to 2007 recorded 38 deaths linked to smoking during oxygen therapy. Alarmingly, 59% of these fires occurred between midnight and 8:00 a.m., a time when people are less alert to potential hazards [43].
Support for Quitting Smoking
Healthcare professionals play a key role in helping patients quit smoking. Without professional help, 90% of people who quit smoking relapse within a year [46].
"Patients don't understand the dangers. If you smoke while using oxygen it can have very serious consequences."
– Beth Grant, Home Oxygen Coordinator Lead, Swansea Bay University Health Board [40]
A combination of behavioural support and medication can significantly improve the chances of quitting. Healthcare providers can develop personalised plans and offer continuous guidance to help patients stay smoke-free [65,58].
Essential Safety Measures
If quitting immediately isn’t possible, there are steps you can take to reduce risks. Always turn off your oxygen tank and wait at least 10 minutes before smoking [44]. Place "NO SMOKING" signs in every room where oxygen is used, and ensure that everyone in your home understands and follows the rules [59,61].
It’s important to note that e-cigarettes and vaping also carry similar fire risks when used near oxygen [41]. Many healthcare providers now recommend home visits to assess safety and ensure compliance, addressing hazards while providing additional education and support.
9. Proven Benefits for Daily Living
Once you've grasped the risks and safety measures, it's time to explore how oxygen therapy can positively impact your daily life. Used as prescribed, home oxygen therapy can enhance energy, mental sharpness, and overall daily activities for individuals with respiratory conditions.
Boosted Physical Activity and Energy
Better oxygen circulation can provide a noticeable energy boost and ease breathlessness during day-to-day activities. Tasks that once felt daunting - like getting dressed, preparing meals, or climbing stairs - become much more manageable. It also opens the door to rediscovering hobbies and interests you may have put on hold [1][2].
Improved Sleep and Mental Sharpness
Using oxygen therapy at night can lead to better sleep and sharper mental focus [2][3][48]. With improved oxygen delivery, your brain - an organ that uses about 20% of your body's oxygen despite making up only 2% of its weight - can function more effectively [51]. This means clearer thinking and better cognitive performance.
Enhanced Social and Emotional Well-being
Oxygen therapy can help restore independence and encourage social interaction [48]. As Eileen M. Mumm, MSN, CRNP, FNP-BC, explains:
"As you navigate the challenges of setting up and using home oxygen therapy, remember it can greatly improve your quality of life as your COPD, pulmonary fibrosis or other lung disease progresses." – Eileen M. Mumm, MSN, CRNP, FNP-BC [50]
By reducing physical strain and increasing energy, many patients find it easier to stay active and engage in social activities. This contributes to a more fulfilling lifestyle and can even help alleviate anxiety and depression [49].
Noticeable Health Benefits
Doctors usually recommend oxygen therapy when blood oxygen levels fall below 88%, while a healthy saturation level is generally 95% or above [1]. Keeping oxygen levels within this range helps your organs work efficiently and boosts your ability to exercise [49]. Research shows that sticking to oxygen therapy plans can lead to significant health improvements, especially in exercise tolerance.
The Importance of Following Your Plan
To fully experience these benefits, it’s crucial to follow your healthcare provider’s instructions [47]. With over 1.5 million people in the United States relying on supplemental oxygen, those who adhere to their treatment plans often report meaningful improvements in their quality of life [47].
10. New Research in Oxygen Delivery Methods
Advancements in oxygen delivery are transforming home oxygen therapy, making it more effective, comfortable, and user-friendly. Building on the established benefits of home oxygen therapy, recent research and innovations are driving significant improvements in patient care and overall experience.
High-Flow Oxygen Systems: A Game Changer
High-flow nasal cannula (HFNC) technology is reshaping oxygen therapy by delivering heated and humidified oxygen at much higher flow rates than traditional systems. High-flow nasal cannula (HFNC) systems are available for severe cases, typically managed in hospital settings or with close medical supervision [54].
"HFNC is able to provide high levels of both oxygen (up to 100% FiO2) and high levels of flow (up to 60 LPM)." – Glen B. Chun, assistant professor, Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, Icahn School of Medicine at Mount Sinai [54]
Research highlights HFNC's effectiveness: a 2015 study revealed that patients with acute respiratory failure had a significantly lower 90-day mortality rate (12%) compared to those using standard oxygen therapy (23%) [54]. Additionally, around 71% of COVID-19 patients treated with HFNC avoided the need for intubation [55].
Smarter Oxygen Delivery with AI
The integration of AI into oxygen concentrators is revolutionising how therapy is delivered. These devices can now adjust oxygen output in real time based on a patient’s respiratory rate and activity levels [56]. Wearable devices, such as advanced pulse oximeters, work in tandem with these concentrators, providing continuous oxygen level monitoring and enabling instant adjustments [52].
Lightweight and Portable Solutions
In January 2024, Inogen, Inc. received FDA approval for a new lightweight oxygen concentrator [53]. This marks a significant step towards making oxygen therapy more portable and convenient. Advances in pulsed flow technology have also made portable devices more energy-efficient, allowing them to operate longer on a single battery charge [52].
Remote Monitoring Through Telemedicine
Telemedicine has opened up new possibilities for oxygen therapy. Healthcare providers can now remotely monitor oxygen saturation levels and make real-time adjustments without requiring patients to leave their homes [56]. This is especially beneficial for individuals with mobility challenges or those living in remote areas.
Market Trends and Future Growth
The oxygen therapy market is poised for substantial growth, with projections estimating it could reach USD 61.08 billion by 2032, growing at a compound annual rate of 6.79% from 2024 to 2032 [53]. The home healthcare segment currently dominates, accounting for 68.65% of the market share, reflecting a broader shift toward home-based treatments [53]. These advancements are not only improving patient care but are also making oxygen therapy more accessible to those who need it most.
Conclusion
These ten key insights equip you to take charge of your respiratory health with confidence. Home oxygen therapy, when used as instructed, can greatly enhance your quality of life. As the American Lung Association explains, "Supplemental oxygen does not cure lung disease, but it is an important therapy that improves symptoms and organ function" [2]. Knowing how oxygen therapy works, practising fire safety, and following prescribed settings are all crucial steps to maximise its benefits.
Safety should always come first. To reduce fire risks, keep heat sources at least 3 metres away from your oxygen equipment, display "No Smoking" signs prominently in your home, and Inform your family members and building security staff that oxygen equipment is in use, so they can assist in an emergency [6]. These precautions ensure not only your safety but also uninterrupted therapy.
Oxygen therapy is typically prescribed when blood oxygen levels fall below 88%, and adhering to the prescribed flow rates is critical for effective treatment [1]. Sticking to these settings ensures you receive the full therapeutic benefit.
Regular maintenance of your equipment is just as important. Experts stress that "regular maintenance of your home oxygen equipment is essential for optimal performance and safety" [26]. This includes cleaning tubing weekly, inspecting for damage, and replacing filters as directed [26]. These steps help prevent malfunctions and extend the life of your devices.
Being aware of low oxygen warning signs allows for timely action. Symptoms like shortness of breath, fatigue, dizziness, and confusion signal a potential issue. Regularly monitoring your oxygen saturation - ideally at 95% or higher - helps you stay within safe limits [1].
The benefits of oxygen therapy go beyond easing breathing difficulties. It can alleviate symptoms like fatigue and shortness of breath, while also improving alertness, sleep quality, and mood [58]. As one caregiver shared, "Both physical and probably emotional. It's, I think for him, it is a feeling of safety: 'I can breathe'" [57].
Success with home oxygen therapy depends on consistent safety practices, routine equipment care, and open communication with your healthcare team. By applying these ten essential principles, you’re not just managing a medical condition - you’re actively improving your respiratory health and reclaiming a better quality of life. Every step you take ensures that your therapy supports your overall well-being.
FAQs
What types of home oxygen systems are available, and how do I choose the best one for my needs?
Home oxygen systems come in a variety of options, tailored to meet different needs and lifestyles:
-
Oxygen Concentrators: These machines draw oxygen from the surrounding air, making them perfect for home use. They run on electricity and provide a steady oxygen supply.
-
Portable Oxygen Concentrators (POCs): Compact and battery-powered, POCs are ideal for those who travel or lead active lives. They typically deliver oxygen in pulses, making them easy to carry around.
-
Compressed Oxygen Cylinders: These are metal tanks filled with oxygen and come in multiple sizes. They work well for both home use and outdoor activities.
-
Liquid Oxygen Systems: These systems store oxygen in liquid form, offering a concentrated oxygen supply without needing electricity. They usually include a stationary unit for home use and a portable tank for convenience when stepping out.
When choosing the right system, think about your prescribed oxygen flow rate, daily habits, mobility needs, and personal preferences. It's always a good idea to consult your doctor to ensure the system aligns with your health and lifestyle needs.
What are the best practices for safely using home oxygen therapy and preventing fire risks?
To ensure the safe use of home oxygen therapy and minimise fire hazards, keep these practical tips in mind:
-
Keep oxygen equipment away from heat sources such as stoves, candles, or electrical appliances. Keep oxygen equipment at least 3 metres away from open flames, stoves, or candles, and at least 1.5 metres from electrical appliances.
-
Prohibit smoking near oxygen. Never smoke or allow others to smoke in the vicinity of oxygen equipment, as it greatly increases the risk of fire.
-
Avoid flammable products like petroleum jelly or aerosol sprays near oxygen, as they can ignite easily.
-
Ensure proper ventilation in the room where oxygen is used to prevent oxygen concentration from building up.
-
Inspect your oxygen equipment regularly for leaks or damage, and follow the manufacturer’s guidelines for safe usage and maintenance.
Following these precautions can make home oxygen therapy safer and significantly reduce fire risks.
What should I do if I feel breathless or notice signs of low oxygen levels while using home oxygen therapy?
If you're feeling breathless or notice signs of low oxygen levels, the first step is to check your oxygen equipment. Look for issues like disconnected tubing, an empty oxygen cylinder, or a power supply problem. Only adjust the device settings if your doctor has specifically advised you to do so.
Should your symptoms continue or get worse, contact your healthcare provider without delay. They might need to review your oxygen therapy or explore other possible reasons for your condition. In situations where symptoms are severe - such as extreme shortness of breath or confusion - don’t hesitate to seek emergency medical assistance. Prioritising your safety is crucial.
Ready to experience safe, hassle-free oxygen therapy at home? Browse our oxygen solutions or contact our 24x7 support team for expert guidance. O2 For Everyone delivers oxygen equipment quickly—often within hours of your request—and provides 24x7 phone and WhatsApp support for setup, troubleshooting, and refills.




 Q. What should I do if someone is turning blue from breathing difficulty?
Q. What should I do if someone is turning blue from breathing difficulty?